*Written for Interactions magazine by Hugh Dubberly, Rajiv Mehta, Shelley Evenson, Paul Pangaro.*
*Editor’s Note:
*
Improving healthcare is a wicked problem [1]. Healthcare’s many stakeholders can’t agree on a solution, because they don’t agree on the problem. They come to the discussion from different points of view, with different frames. Wicked problems can be “solved” only by reframing, by providing a new way of understanding the problem that stakeholders can share [1]. This article describes a growing trend: framing health in terms of well-being and broadening healthcare to include self-management. Self-management reframes patients as designers, an example of a shift also occurring in design practice—reframing users as designers. The article concludes with thoughts on what these changes may mean when designing for health.
*—Hugh Dubberly*
**What is health?**
From the point of view of today’s healthcare system, health is largely about minimizing illness. The healthcare system has evolved primarily for treating acute conditions. Despite flaws (including high cost and limited access), the system does a good job of curing infections, repairing injuries, and responding to emergencies. The healthcare system does less well in treating chronic conditions. It provides resources for managing aspects of systemic problems, such as statins for cholesterol, ARBs and ACE inhibitors for high blood pressure, and insulins for diabetes; but in most cases that means merely slowing the rate of decline. Yet health is “not merely the absence of disease or infirmity.” In contrast, the World Health Organization defines health as “a state of complete physical, mental and social well-being” [2].
Health as well-being depends not just on healthcare but also on employer practices [3], social policies [4], and self-management, the main subject of this article. Of course, health is “not the objective of living”; health is a resource contributing to the quality of our everyday living [5].
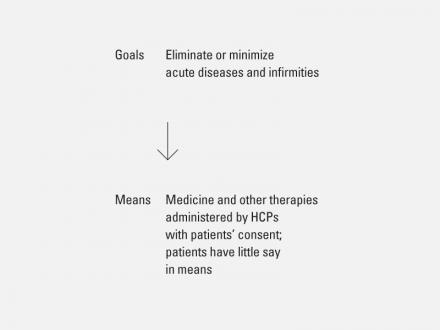
Traditional healthcare focuses on treating acute problems.
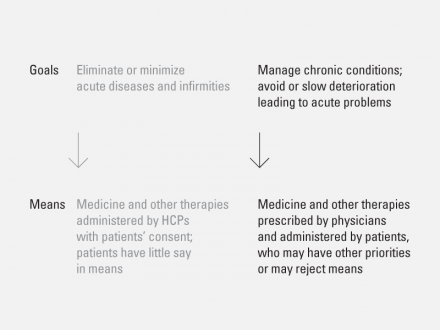
Traditional health management applies the tools of acute care to stabilizing chronic conditions.
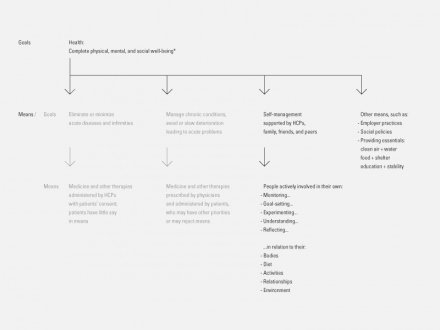
Health is more than eliminating or managing disease; and its requirements extend beyond traditional healthcare.
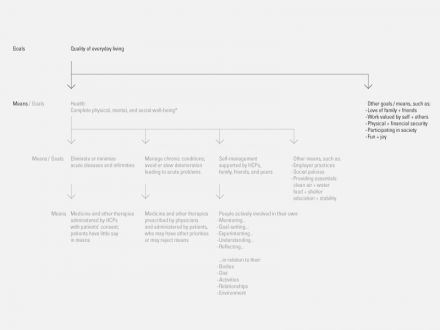
Health is a means to higher goals — “a resource for everyday life, not the objective of living” — World Health Organization (WHO)
**Identifying the Frame of Healthcare**
The way we usually think about health today is bound up in the language of our healthcare system. We call individuals “patients.” We call physicians healthcare “professionals” (HCPs). Professionals “care for” patients—by observing symptoms, diagnosing diseases, and proposing therapies. Their proposals are not just suggestions; they are prescriptions or literally “physician orders.” Patients who don’t take their medicine are not “in compliance.”
In the relationship between HCPs and patients, HCPs dominate. HCPs do whatever is necessary, with patients playing a relatively passive role [6]. In some ways, the system reduces patients to the status of children—simply receiving treatment. The power imbalance may grow out of illness. When we feel ill, we may seek comfort or aid from others. When we feel afraid, we may hand responsibility to a confident expert. In a medical emergency, letting a physician take charge is probably the surest way to stabilize things and return to normal.
A heart attack requires quick action; it’s not the best time for discussion. The time for discussion is before a heart attack occurs—and after—finding ways to avoid the heart attack in the first place or at least avoid another one.
Yet the language of acute conditions (the frame of healthcare) is ill suited to managing chronic conditions or preventing disease (often framed as behavior change). The American Heart Association reports, “The No.1 problem in treating illness today is patients’ failure to take prescription medications” [7]. Patient behavior does not change on a physician’s orders. To expect behavior change on command is to misunderstand human nature. To blame patients (who respond to the very present pressures of busy lives rather than less tangible long-term risks) is unhelpful, unkind, and perhaps unethical. (Blaming patients—or clients—suggests that one doesn’t understand or respect their context and constraints and doesn’t share responsibility for outcomes.) According to social epidemiologist Leonard Syme, “We need to pay attention to the things that people care about, and stop being such experts about our risk factors” [8].
The language of acute conditions (the frame of healthcare) limits what we imagine. Discussions about improving healthcare focus mainly on improving assessment of patient conditions, improving HCP education, and improving therapies—since surviving a crisis depends mainly on the patient’s condition, the HCP’s skill, and the medical technology at hand.
We debate how to have more of the same rather than something new. We debate how to be more efficient and reduce cost rather than radically increase effectiveness and eliminate causes. Our goals remain modest. We seek little more than increased patient compliance and more knowledgeable consumers. We can do better.
The language of acute conditions (the frame of healthcare) is ill suited to achieving well-being (the frame of self-management). By its very definition, healthcare almost assumes both a present problem and an expert who intervenes. In that sense, well-being lies outside the scope of our current healthcare system. Wellness is more than absence of illness: It’s is a way of living. Well-being requires its own language, its own frame.

Self-management does not replace healthcare; rather it acknowledges the limits of what healthcare can accomplish and seeks structures that go beyond those limits.
**Imagining the Frame of Self-management**
Foucault attributes “the birth of the clinic” to the Enlightenment, when early versions of the current healthcare paradigm displaced a medieval paradigm [9]. The language of health had a beginning; it was invented. And like other languages, it can evolve; we can reinvent it [10].
Imagine reframing health so that it includes self-management.
Self-management suggests a fundamental shift of responsibility. Patients reclaim their role as adults responsible for their own well-being. The relationship between HCP and patient becomes more symmetric (at least outside of medical emergencies). Issuing orders gives way to discussing and collaborating. HCPs become coaches and assistants, shifting their stance from dispensing knowledge to learning from patients. As Melanie Swan reports, “a collaborative co-care model is starting to evolve for healthcare delivery…the patient’s role may become one of active participant, information sharer, peer leader and self-tracker, while the physician’s role may become one of care consultant, co-creator and health collaborator” [11].
In the parlance of “design for service,” HCPs begin to think of themselves as “co-producing” health and well-being with their patients. Imagining healthcare as a designed service is another way to reframe it. Kaiser and the Mayo Clinic employ design innovation teams; UPMC has teamed with CMU design students to reimagine patient experiences [12].
Self-management also suggests setting goals and measuring progress—the basis for managing and improving quality. Individuals decide what’s important to them, what well-being means, what they want to work on. Individuals record their actions; for example, meals eaten, exercise completed, medications taken, hours slept, time spent working or playing or commuting, and perhaps even interactions with others and media consumed (e.g., music played). Individuals also measure results; for example, hard values such as their weight, pulse, blood pressure, cholesterol, and blood glucose; and softer values such as energy, stress, pain, happiness, or mood.
Then they repeat the cycle. If they’ve made progress toward their goals, they may continue the same course of action or even speed up. If they’re diverging from their goals, they may change course. Individuals find and maintain a “healthy balance,” one that’s comfortable for them. They take an active role in their body’s process of homeostasis—including physical, emotional, and social dimensions.
This process is directed trial and error—experimenting, something like the Shewhart-Deming PDCA cycle, a simple application of the scientific method, a version of the design process.
Imagine patients as designers—conducting billions of tiny self-experiments, prototyping their own well-being. That’s the essence of a self-management approach to health [13].
Far-fetched? An impossible change?
**Emerging Trends Support Self-management**
Self-management has always existed. Americans spend billions of dollars each year on health foods and diet programs. A doctor reported, “20% to 30% or my patients are into some type of supplements or ‘nutraceuticals’” [14]. Deloitte reported that 20 percent of consumers used alternative therapies [15]. Kaiser reported that 33 percent of consumers had “relied on home remedies or over-the-counter drugs instead of seeing a doctor” in the past 12 months because of cost concerns [16].
Several factors have begun the process of reframing health as self-management. The U.S. healthcare system is out of control; managing costs requires a focus on what the medical profession calls outcomes. The public has a growing awareness that well-being is more than healthcare. The fitness and exercise movement, elements of the DIY (Do-It-Yourself) movement like [the Quantified Self group][1], behavior-change programs like Weight Watchers, and more progressive programs for managing chronic conditions like the Stanford Cardiac Rehabilitation Program [17], all point the way to self-management.
The shift to self-management is also supported by changes in the Internet and related technologies. Melanie Swan reported, “Individuals are becoming more engaged in a variety of self-testing and self-management of conditions, symptoms, genomics and blood biomarkers, behaviors and personal environmental factors. Individuals could dramatically expand their use of web-based tools, devices and health-based social networking platforms as their awareness increases, costs drop, financial incentives arise and automated tools proliferate” [11]. The Internet and related technologies are also making it easier for people to have conversations that support self-management.
Imagine online social-network applications creating communities of support around diseases, chronic conditions, and fitness. Of course, health-based social networks have already begun; what’s surprising is just how many there are [18]. Other social network applications serve broader audiences while also offering health-related components [19].
Social networks are dynamic; they can generate collective action. In addition to individuals experimenting on themselves, groups of people with similar conditions—people joined together through online social networks—may sponsor or conduct research. Already, online social networks have begun to affect clinical trials, helping researchers find participants and helping participants compare outcomes.
Imagine several sensors monitoring each person. Already nearly continuous monitors are available for pulse, steps walked, and blood glucose, at relatively low cost. More types are on the way. Many of these sensors send data to the Internet, either directly or through mobile devices or desktop computers, which forward the data. Withings sells a Wifi Body Scale that sends your weight to Twitter each time you weigh yourself [20].
The sensor revolution will change the way we view data and ourselves. Children born in the next decade may look back across a lifetime of data. We won’t be able to ignore how we’re doing; we’ll always know. Continuous feedback may provide micro-motivation—the ongoing awareness we need to live healthier lives.
Imagine personal-health dashboards, applications for tracking your sensor data based on the Web or mobile phones. (Your mobile phone may become a server at the hub of your body-area network.) Health dashboards will provide trend graphs, comparisons with goals and norms, and alerts when things change suddenly or move toward unsafe levels. Health dashboards will be just one of several dashboards in our lives, including those for finance like mint.com, home networks like Pie Digital, and home energy management like the demo Intel showed at CES 2010. In a way, social-network sites, like Facebook, are also dashboards—for friends and message management. Health-based social networks and personal health dashboards seem likely to combine and reinforce one another.
Imagine big data-mining software learning from all the data stored in health dashboards. (Big data is computer-industry jargon for huge databases of information generated on the Web; data mining is jargon for the process of correlating data to generate value. Google’s page-rank algorithm, which bases relevance on counting links to a Web page, is a classic example of big data mining.)
Data that individuals collect will establish a baseline for comparing future measurements. Identifying personal norms is important, especially when we’re not average. For some, 98.6 may indicate a fever, especially as normal body temperature decreases with age. Collecting data will also enable individuals to compare themselves to others—to the entire population or to those sharing similar characteristics, such as age, sex, height, weight, conditions, genes, environment, and even behavior.
Ian Shadforth points out that once health data collecting begins in earnest, we can quickly generate population-wide norms and norms for many sub-groups. By collecting data on a range of age groups simultaneously, we may need just a few years to generate a picture of what’s “normal” across a lifetime [21].
The growth of online health-based social networks, bio-medical sensors, personal health dashboards, and health-focused big data mining applications will not of themselves or even in combination force a shift to self-management. They simply make measurement and tracking a lot easier. They lower the bio-cost of self-management. And they make visible—perhaps even cool—the practice of measurement and tracking. In this way, technology may set off a process of bootstrapping, which can lead to the broader changes we describe.
**Parallels with Changes in Design Practice**
Reframing health as self-management parallels similar trends in education, where we increasingly recognize that students manage (or design) their own learning, and design practice, where we increasingly recognize that users manage (or design) their own experiences. Perhaps these changes are part of larger trends, the democratizing of professionalism and the shift from a mechanical-object ethos to an organic-systems ethos [22].
Good teachers do more than pass on facts; they help students learn how to learn, so that teaching becomes what Paulo Freire calls the “practice of freedom,” a means to deal critically with one’s living and discover how to transform the world [23].
Freire also insisted on symmetry in the relation between teacher and student—or at least “deep reciprocity.” (Good teachers learn from their students.) Freire’s position echoes Horst Rittel’s assertion that the participants in a design project (all the stakeholders including professional designers) share a “symmetry of ignorance” (or knowledge) regarding the problem. Rittel’s point is that design problems are always “owned” by someone [1]. Design problems have no objective definition; their definition reflects the owner’s point of view. Here, Rittel challenged the orthodoxy of professional problem solving and opened the door to the design process, inviting users and other stakeholders to step inside.
The 1990s saw the flowering of user-centered design. Ethnography and other forms of research about users became standard practice in software design.
Some professional designers began to see their work as engaging stakeholders in a discussion. Liz Sanders and others have begun to advocate for participative design and co-creation—not just designing for users, but designing with them. Co-production has become a watchword in the emerging field of service design (or design for service), as designers recognize the integral role of “consumers” in producing services.
Shelley Evenson and others talk about creating conditions in which users become designers—creating spaces in which people can learn and grow. That means professional designers become meta-designers, designing open-ended systems, languages, platforms, APIs, construction kits, or kits of parts, which others configure or re-configure to their own ends. Wooden blocks, Legos, and train sets are classic examples, kits of parts with which we may play—and design. Herman-Miller’s Action Office is a kit of parts designed for others to design offices. (Sadly, it gives little design control to the office’s occupants.) Programming languages and code libraries like Java and Flash are kits of parts for others to design software. (How much design control can the resulting applications give end-users?) Even simple services like restaurants offer a menu of choices from which patrons may design a dish or a meal. Starbucks and Mini-Cooper offer a dizzying array of choices from which customers can design.
As with health (and education), reframing design will not be easy. For designers who have spent years perfecting their craft and who delight in making beautiful form, the notion of user as designer and designer as facilitator can seem frighteningly foreign. Yet this transition offers the opportunity to make the world richer—to create more options for everyone, including professional designers (and HCPs and teachers).
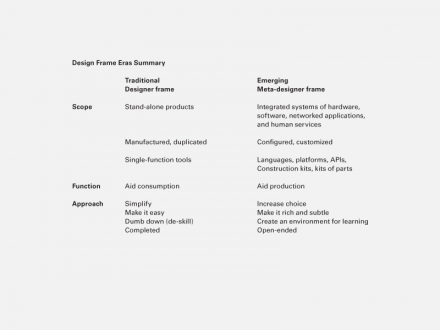
As the era of mass production ends, design practice must adapt to the new era of information. In order to create value, designers will increasingly have to frame their work in new ways.
**Design for Health**
As healthcare becomes a larger part of the economy and as healthcare practice and research biology both converge with computing, opportunities to design software and services for health abound. We should keep in mind that health is a means to a goal—one of the things that supports the quality of our everyday living.
Designers should ask their clients: How should we frame health in this engagement? Are we bound to the frame of traditional healthcare? Or can we apply a broader frame, such as self-management?
Designers should also ask themselves and their colleagues: How should we frame design in this engagement? Are we designing artifacts or services? Where might we create opportunities for users to design?
If the user is both designer and implementer (combining first- and second-order agency), what is possible? How can we help users act? Track results? Set goals? How do we “scaffold” tiny self-experiments, learning, and sharing?
Designers should also help users discover and understand both the short-term relationship between action and result (incremental changes that the individual can actually make) and the long-term consequences (big outcomes that matter over time).
Creating opportunities for users to design requires not only giving them responsibility for means and goals but also enabling conversations for:
+ overcoming the barriers (bio-cost) of making incremental change through…
+ making results, trends, and projections visible and…
+ providing emotional support (such as family and community engagement) to maintain…
+ higher-level strategic views of the entire process, to maintain goals and momentum, that in turn…
+ create learning across time and circumstances that can be shared…
+ improving the system for others
We’re on the brink of something new—the intersection of health and computing, design and service. What will we invent as these processes converge? What happens when health self-management meets meta-design?
**About the Authors**
Hugh Dubberly manages a consultancy focused on making services and software easier to use through interaction design and information design. As vice president, he was responsible for design and production of Netscape’s Web services. For 10 years he was at Apple, where he managed graphic design and corporate identity and co-created the Knowledge Navigator series of videos. Dubberly also founded an interactive media department at Art Center and has taught at CMU, IIT/ID, San Jose State, and Stanford.
Rajiv Mehta consults on exploring and commercializing radical innovation, driving ideas from concept to market. His work has ranged from photography to lasers, computer vision to wireless, and health, at companies from Adobe and Apple to Symbol Technologies and Zume Life. He studied at Columbia, Stanford and Princeton.
Shelley Evenson recently joined Microsoft’s FUSE (Future Social Experience) Labs as a principal in user experience design. Before FUSE, Shelley was an Associate Professor teaching interaction design at Carnegie Mellon University. Shelley taught courses in designing conceptual models, interaction, and service design, and collaborated in projects with colleagues from the Tepper School of Business and the Human Computer Interaction Institute. Shelley jumpstarted the study of service design in the U.S. designing courses, energizing students, and hosting the first international conference on service design-Emergence. Before joining the faculty at Carnegie Mellon University, Shelley worked for more than 25 years in multidisciplinary consulting practices, working with on a wide variety of design and development projects.
Paul Pangaro is the CTO at CyberneticLifestyles.com in New York City, most recently working for clients in consumer internet and mobile computing. He has designed a search engine for poetry, interactive information strategies for medical services, and a framework of ontogenetic sharing for social networking. Paul has lectured at London’s Bartlett School of Architecture, São Paulo’s Instituto Itaú Cultural, École Nationale Supérieure des Mines de Paris, and MIT’s Media Lab and Sloan School of Management on design process, conversation theory applied to interaction design, and the cybernetics of innovation. He was CTO of several startups, including Idealab’s Snap.com, and was senior director and distinguished market strategist at Sun Microsystems. Paul has taught at Stanford University and teaches in the MFA program on interaction design at the School of Visual Arts, New York City.
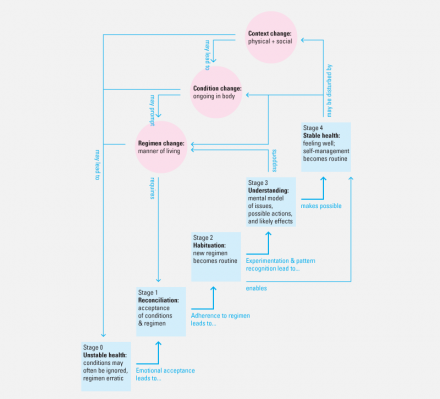
Continuous Cycle of Health Self-management.
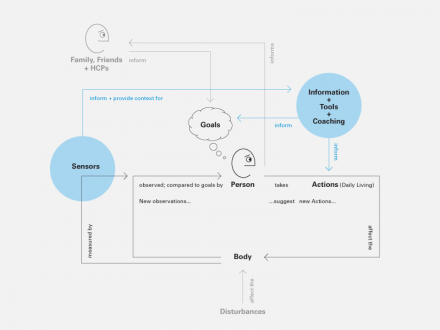
Self-arrangement augmented by conversation with others, sensors, and services.
[1]: http://www.quantifiedself.com/ “the Quantified Self group”
4 Comments
Simon Reynolds
Oct 24, 2010
11:24 pm
Great work.
It is good to see others who recognise this need.
Software as service innovation in self organisation.
Regards
Simon Reynolds
Health and Fitness Article
Oct 30, 2010
12:17 pm
We need to focus more on prevention of disease. This is an area that our present system falls short.
Haig Bedrossian
Mar 8, 2011
9:47 am
Putting design to humanitarian uses, is good for the planet.
Chris Byers
Nov 20, 2020
10:52 pm
Love this! Thank you for sharing!